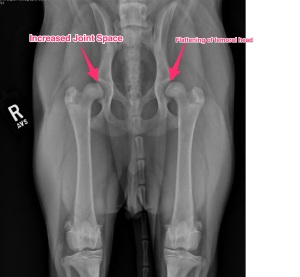
After the diagnostics were performed (reviewed in the previous segment), a decision needed to be made as to which issue was to be addressed first. This is often a tough decision and must be made with the experience of your trusted veterinarian. My criteria consisted of which leg was most affected and the fact that I had already decided to address his hips with a total hip replacement. In my opinion (and supported clinically), a total hip replacement was a better option than other procedures available for canine hip dysplasia. Certain growth plates (centers of bone growth) need to be closed prior to performing a total hip replacement making the minimum age being around 10 months of age. This made our decision easier and the decision to address the elbows was made.
Surgery for his elbows was staged; the left elbow surgery performed on December 6, 2013 and the right elbow addressed on February 14, 2014 (Happy Valentine’s Day!). The time period in between was used for physical therapy and maximizing the results of the surgeries. Identical surgeries were performed on both elbows due to the similarity of the disease process occurring. An elbow arthroscopy was performed, which revealed the cartilage flap (osteochondritis dissecans (OCD)) and a fragmented coronoid process (FCP) The OCD flap was removed and the FCP segment was removed. The damaged bone under the OCD flap was removed with a shaver until healthy bone was present. Since the diseased area of the elbow was on the inside (medial) aspect a specialized procedure to displace weight to the central and outside (lateral) aspects was performed. This procedure is called a sliding humeral osteotomy (SHO). This procedure is fairly aggressive and involves a bone cut in the middle of the humerus bone and a plate/screws placed.
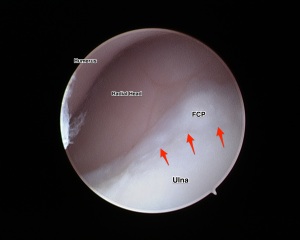
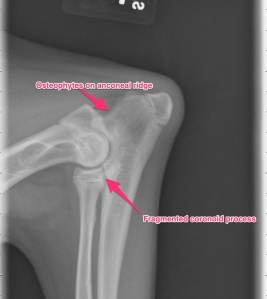
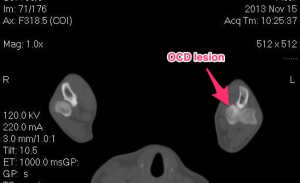
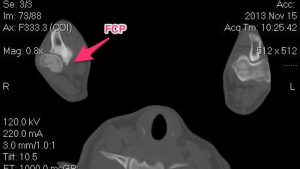
Below are images of the elbow arthroscopy showing both the OCD lesion and the FCP segment.

Note the underlying bone (pink). This is usually covered by cartilage, however the cartilage has become a flap.
Following the elbow arthroscopy, the SHO procedure was performed. Below is a radiograph of the procedure.