While the thought of a total hip replacement can conjure up thoughts of discomfort, pain and prolonged recovery, most of the time this is not the case. In dogs, total hip replacements have been performed for over 25 years and typically have great success when performed by the experienced surgeon with an experienced team. There are many reasons for total hip replacements in the dog, but the most common reason is as a treatment for canine hip dysplasia.
When considering whether a total hip replacement may be an option for your pet, a consultation with a boarded veterinary surgeon who is experienced in this procedure is the first place to start. Typically your family veterinarian can guide you in this process and make a referral to a surgical center that they trust. When you are faced with this possible treatment option, you will be overwhelmed with questions and the biggest being, “is this the right thing to do for my pet?” My goal is to try to answer some of the commonly asked questions by owners. While I may be biased since I am a veterinary surgeon, I have also been on the owner side of the equation with my own dog with bilateral hip dysplasia (see Frankie’s Journey).
What are the common indications (reasons) why a total hip replacement would be recommended?
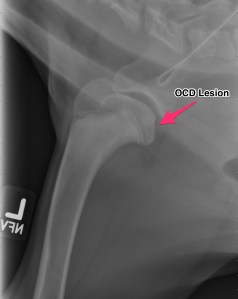
This is one of the biggest questions that I hear and there are actually many reasons that a total hip replacement may be recommended. The most common reason is chronic hip dysplasia. While we see hip dysplasia less than a few decades earlier, we do still see this potentially debilitating disease with some frequency. Hip dysplasia refers to a hereditary issue that induces laxity (looseness) within the hip. This looseness causes subluxation or luxation of the affected hip. Subluxation refers to movement of the femoral head partially out of the acetabulum. Think of a ball and socket joint and the ball(femoral head) is popping out of the socket(acetabulum) with movement. Luxation refers to the femoral head completely coming out of the acetabulum. This alone can cause pain and lameness in puppies and young dogs. In some dogs, they learn to navigate without much discomfort, but the joint will start to develop chronic arthritic changes and cartilage wear that go on to cause pain and discomfort. While we term a total hip replacement an end stage procedure, this just means that in dogs with chronic hip dysplasia and arthritis we always try medical/conservative management prior to surgery. There are dogs that, despite medical management and rehabilitation, are still painful and require surgical intervention; or dogs that need to be on medications continuously for the rest of their lives to be comfortable which would also qualify as a total hip replacement candidate.

Frankie’s pre-operative x-rays. Bilateral hip dysplasia.
Other indications for a total hip replacement would include fractures associated with the hip, especially when associated with the femoral head and neck. Traumatic hip luxations are another indication. This is where the hip “pops” out of the joint due to excessive force, such as a dog that has been hit by a car. We do see congenital, chronic hip luxations and acute, non-traumatic luxations, however these cases tend to be at a heightened risk of complications with a total hip replacement. Your surgeon will review the options if your dog has this type of condition. Another indication would be for avascular necrosis of the femoral neck – this is a condition where the blood supply to the femoral neck is altered and reduced during the growth phase. Subsequently the femoral neck and head undergoes cell death (necrosis) which leads to deformation and eventual fracturing. This is more commonly seen in small breed dogs.
What types and sizes of dogs are candidates for a total hip replacement?
We generally think of total hip replacement for larger dogs, which used to be the case. The typical dogs that receive this type are surgery are the retriever and shepherd breeds, since we see hip dysplasia in these dogs more commonly. The standard weights of dogs tend to be 40 pounds and over, however that is changing. With the onset of smaller instrumentation and implants, we now can implant a total hip replacement in a dog as small as five pounds and in some cats.
Isn’t my dog too young for a total hip replacement?
While there are certain age related requirements, there aren’t any exact age requirements. Most of the requirements are based on growth plate closure associated with the femur and in particular the greater trochanter, which generally is closed at around 9-10 months of age (older in giant breed dogs). Some clients will ask, “isn’t my one year old Golden Retriever too young?” My response is “no” if the patient is painful and not responding to the conservative management. The implants themselves have a life span of >15 years, generally exceeding the life expectancy of the pet.
The converse of whether the pet is too young for a replacement is the questions as to whether the pet is too old for the procedure. With older dogs, we need to look at the entire health of the patient and ensure that the patient does not have any other related or unrelated illnesses. Total hip replacements still may be recommended in our geriatric patients.

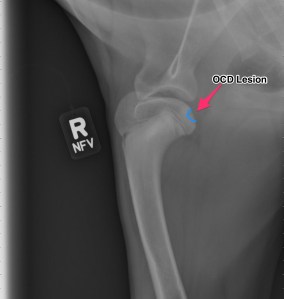
Frankie’s post operative radiographs. Left total hip replacement.
What should I expect on my initial consultation for a total hip replacement?
Every surgeon conducts their examinations differently, so here is a brief overview of a standard consultation that I would perform. Obtaining an accurate history is imperative, so be sure to be upfront with what you are seeing at home, when lameness started, what side is most affected, and ALL medications that your pet may be on or may have tried in the past related to treating lameness.
A full physical examination will be conducted looking at general health, orthopedic and neurologic health. During the general examination we are looking for any other issues that may be just as or more important than your pet’s lameness. Some examples are dental disease (potential infection source), heart murmur/cardiac disease, masses palpated on skin, abdomen or on rectal examination, and skin health. Skin infections (even mild) NEED to be treated prior to surgical consideration due to implants being used.
A full orthopedic exam is needed to rule out any other common orthopedic disease such as cranial cruciate ligament (ACL) tears, medial patella laxations, etc., which may require surgical treatment before considering a total hip replacement. A complete neurologic examination is also needed as neurologic disease would be cause for concern.
Below is a summary of the initial consultation:
– Complete examination
– Sedated X-rays. Most patients (even the best behaved patients) will require sedation for radiographs (x-rays) of the hips. We use these x-rays for measurements of implants, so they must be PERFECT. Remember that the reason your pet is seeing a surgeon is because of hip pain, and the positioning of the x-rays may cause some discomfort, so the kindest way to acquire radiographs is with sedation.
– Blood work: Complete Blood Count (CBC), Chemistry profile, and Urinalysis. This needs to be performed at the MOST 30 days prior to surgery to ensure that your pet is a good anesthetic candidate.
– In older patients, additional diagnostics may be recommended such as chest radiographs and an abdominal ultrasound to get a complete health screen.
Assuming your pet is a good candidate for a total hip replacement the procedure will be described to you in detail along with the potential complications, recovery period/rehabilitation, and overall outcome. If for some reason a total hip replacement is not a good choice or another issue is found, other treatment options will be reviewed in depth. I always mention to owners to allot enough time for the consultation since a lot is performed on that first visit.
Will both hips need a replacement?
Every surgeon may have a differing of opinions on this. My thoughts reflect the more conservative viewpoint of 20% of dogs with disease in both hips, need hip replacements in both hips. We tend to see a large amount of patients compensating very well when one hip is replaced. That being said there are some dogs that do require both be performed. The typical time frame for performing surgery on the second side is about six months (sooner in a small number of patients).
Are there other hip procedures other than a total hip replacement?
There are four main surgeries available for hip dysplasia in the dog. The first two have strict time frame/age requirements. The first is called a Juvenile Pubic Symphodesis (JPS) which is a procedure that fuses a growth plate that allows the acetabulum (cup/socket) to cover the femoral head (ball) better. This must be performed in dogs under 6 months of age, before the growth plate closes on it’s own. The second procedure is called a Double/Triple Pelvic Osteotomy (DPO). This is performed ideally in dogs under 10-12 months of age and prior to development of any arthritis. This procedure improves the coverage of the acetabulum over the femoral head and can be very effective in dogs with subluxation rather than luxations.
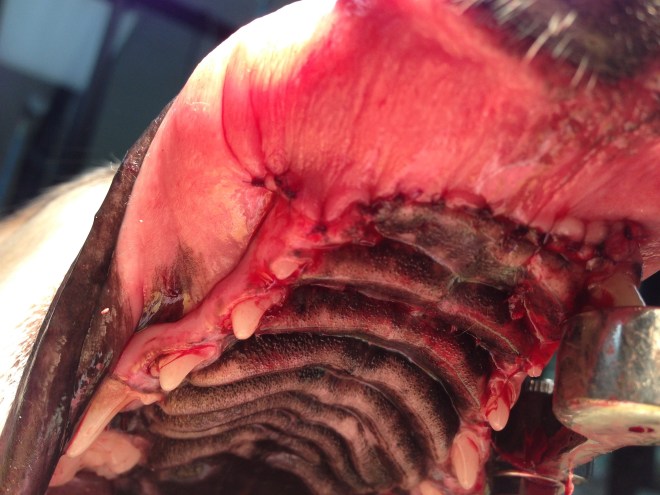
The two main surgical interventions for adult dogs with hip dysplasia are the Total Hip Replacement (THR), which is the scope of this article and the Femoral Head Ostectomy (FHO). The femoral head ostectomy is a procedure where the femoral head is removed and not replaced. This removes the painful source of the femoral head as it contacts the surface of the acetabulum. This is performed with a degree of frequency in small breed dogs and cats, but is considered in some cases of larger breed dogs. There are some cases where this procedure is the best option, however it has been seen that overall use and function of the limb is diminished when compared to a successful total hip replacement. In some studies, an unsatisfactory result (decreased range of motion and decreased muscle mass) has been described in as high as 40% of cases where a FHO was performed.
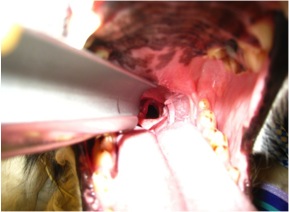
The total hip replacement is a procedure that replaces both the femoral side (femoral head and neck) and the acetabulum. This procedure when successfully performed allows for normal, uninhibited movement of the new hip and generally allows for a full recovery. This procedure has been done in many working dogs (police dogs, service dogs, etc.) in which the dog is able to resume its normal “job”.
Are “cementless” implants better than “cemented” implants?
There are definitely pluses and minuses to both systems. “Cementless” implants are also thought of as press fit and have a surface where the bone grows into the implant. “Cemented” implants are held in place by a polymerizing bone cement and is as strong as it will be once it solidifies and dries. We do see a slightly higher risk of infection around the implants with the cemented implants as well as what is termed “aseptic” loosening. Where the bone anatomy allows, we strive to use the “cementless” implants.
What are the potential risks and complications that could occur after a total hip replacement?
During the initial consultation we always cover potential complications. While the total hip replacement procedure has a high success rate, there are always potential complications. The first type of complication would involve implant complications, which can be exacerbated if the post-operative instructions are NOT strictly followed. Our patients, after all, are dogs and will not regulate their activity appropriately, herein lies the owner’s responsibility. If the patient is too active the more common type of complications are implant shifting, luxation of the hip, fracturing of the femur, femoral stem subsidence, and seroma formation. The first three complication would require another surgery. Other complications could include infection (short and long term), aseptic loosening of the implants, etc.
What is the outcome for my pet after a total hip replacement?
In general, the outcome for the total hip replacement patient is quite good. Ideally the success rate of total hip replacements in the appropriate patient is around 92-95%. The return of function is typically very good and restoration of normal range of motion and improved musculature. The typical recovery/rehabilitation period is about 3 months in total, however it is a gradual ramping up of activity. As I tell my owners, if I can do it with my own dog, you can do it!!
– Frankie one day after a total hip replacement.
– Frankie (and Vinnie) 1 and 1/2 years after his total hip replacement.