Here are some of the diagnostics that were performed on Frankie. As mentioned before, during his first visit a thorough examination was performed, which revealed congenital issues on all limbs. Also, when he presented he was overweight (for a 6 month old puppy). We do know that too rapid growth and obesity at a young age can preferentially express the genes responsible for these issues and exacerbate signs.
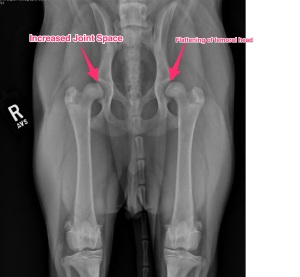
Here are his physical exam findings: lameness noted in all limb, more pronounced on his left side. Pain on hyperextension and hyperflexion of both elbows and pain on palpation of the medial (inside) compartment of both elbows. Pain on hyperextension and hyperflexion of both hips. Positive Ortolani tests on both hips – this is were the femoral head portion of the hip can be pushed out of the acetabulum (socket) and then falls back in; I have downloaded a video displaying this on Frankie.
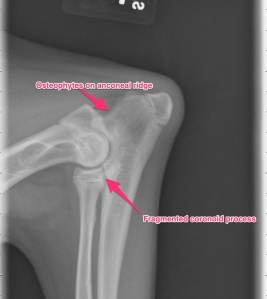
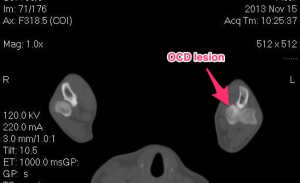
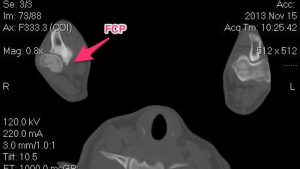
Our first steps in diagnosis was to perform radiographs (x-rays) and a CT scan of the elbows. The x-rays confirmed both elbow dysplasia and hip dysplasia. Interestingly, Frankie had bilateral Osteochondritis Dissecans lesions, which isn’t commonly seen, but can be a part of elbow dysplasia.
The CT scan demonstrates the same lesions as the x-rays, but gives a different view. A CT scan is a very sensitive diagnostic test for elbow pathology, especially in cases that have not developed normal x-rays changes yet.