Take a look at our new Total Hip Replacement (THR) video. This happy dog is a recent (last fall) recipient of a total hip replacement at AVS Orange Park. As you can see, he is a very happy boy and much happier now that he is feeling better!! Please contact us with questions or if you feel that your dog may benefit from a THR.
dogs
Welcome
Welcome to “A Veterinarian’s Perspective”. Thank you for taking the time to visit this site. One of the many goals is to give accurate and useful information about a wide array of veterinary medicine topics. There are many places online one can obtain information; some “good” and some “not so good”. This site is geared to both the veterinary professional and the non-veterinary trained. Another passion and new facet to this website/blog is in the realm of business management as it pertains to the practice of veterinary medicine. Look for some fresh, useful topics in the near future. By all means, feel free to give suggestions for topics!
When to Consider a Total Hip Replacement???

While the thought of a total hip replacement can conjure up thoughts of discomfort, pain and prolonged recovery, most of the time this is not the case. In dogs, total hip replacements have been performed for over 25 years and typically have great success when performed by the experienced surgeon with an experienced team. There are many reasons for total hip replacements in the dog, but the most common reason is as a treatment for canine hip dysplasia.
When considering whether a total hip replacement may be an option for your pet, a consultation with a boarded veterinary surgeon who is experienced in this procedure is the first place to start. Typically your family veterinarian can guide you in this process and make a referral to a surgical center that they trust. When you are faced with this possible treatment option, you will be overwhelmed with questions and the biggest being, “is this the right thing to do for my pet?” My goal is to try to answer some of the commonly asked questions by owners. While I may be biased since I am a veterinary surgeon, I have also been on the owner side of the equation with my own dog with bilateral hip dysplasia (see Frankie’s Journey).
What are the common indications (reasons) why a total hip replacement would be recommended?
This is one of the biggest questions that I hear and there are actually many reasons that a total hip replacement may be recommended. The most common reason is chronic hip dysplasia. While we see hip dysplasia less than a few decades earlier, we do still see this potentially debilitating disease with some frequency. Hip dysplasia refers to a hereditary issue that induces laxity (looseness) within the hip. This looseness causes subluxation or luxation of the affected hip. Subluxation refers to movement of the femoral head partially out of the acetabulum. Think of a ball and socket joint and the ball(femoral head) is popping out of the socket(acetabulum) with movement. Luxation refers to the femoral head completely coming out of the acetabulum. This alone can cause pain and lameness in puppies and young dogs. In some dogs, they learn to navigate without much discomfort, but the joint will start to develop chronic arthritic changes and cartilage wear that go on to cause pain and discomfort. While we term a total hip replacement an end stage procedure, this just means that in dogs with chronic hip dysplasia and arthritis we always try medical/conservative management prior to surgery. There are dogs that, despite medical management and rehabilitation, are still painful and require surgical intervention; or dogs that need to be on medications continuously for the rest of their lives to be comfortable which would also qualify as a total hip replacement candidate.
Other indications for a total hip replacement would include fractures associated with the hip, especially when associated with the femoral head and neck. Traumatic hip luxations are another indication. This is where the hip “pops” out of the joint due to excessive force, such as a dog that has been hit by a car. We do see congenital, chronic hip luxations and acute, non-traumatic luxations, however these cases tend to be at a heightened risk of complications with a total hip replacement. Your surgeon will review the options if your dog has this type of condition. Another indication would be for avascular necrosis of the femoral neck – this is a condition where the blood supply to the femoral neck is altered and reduced during the growth phase. Subsequently the femoral neck and head undergoes cell death (necrosis) which leads to deformation and eventual fracturing. This is more commonly seen in small breed dogs.
What types and sizes of dogs are candidates for a total hip replacement?
We generally think of total hip replacement for larger dogs, which used to be the case. The typical dogs that receive this type are surgery are the retriever and shepherd breeds, since we see hip dysplasia in these dogs more commonly. The standard weights of dogs tend to be 40 pounds and over, however that is changing. With the onset of smaller instrumentation and implants, we now can implant a total hip replacement in a dog as small as five pounds and in some cats.
Isn’t my dog too young for a total hip replacement?
While there are certain age related requirements, there aren’t any exact age requirements. Most of the requirements are based on growth plate closure associated with the femur and in particular the greater trochanter, which generally is closed at around 9-10 months of age (older in giant breed dogs). Some clients will ask, “isn’t my one year old Golden Retriever too young?” My response is “no” if the patient is painful and not responding to the conservative management. The implants themselves have a life span of >15 years, generally exceeding the life expectancy of the pet.
The converse of whether the pet is too young for a replacement is the questions as to whether the pet is too old for the procedure. With older dogs, we need to look at the entire health of the patient and ensure that the patient does not have any other related or unrelated illnesses. Total hip replacements still may be recommended in our geriatric patients.
What should I expect on my initial consultation for a total hip replacement?
Every surgeon conducts their examinations differently, so here is a brief overview of a standard consultation that I would perform. Obtaining an accurate history is imperative, so be sure to be upfront with what you are seeing at home, when lameness started, what side is most affected, and ALL medications that your pet may be on or may have tried in the past related to treating lameness.
A full physical examination will be conducted looking at general health, orthopedic and neurologic health. During the general examination we are looking for any other issues that may be just as or more important than your pet’s lameness. Some examples are dental disease (potential infection source), heart murmur/cardiac disease, masses palpated on skin, abdomen or on rectal examination, and skin health. Skin infections (even mild) NEED to be treated prior to surgical consideration due to implants being used.
A full orthopedic exam is needed to rule out any other common orthopedic disease such as cranial cruciate ligament (ACL) tears, medial patella laxations, etc., which may require surgical treatment before considering a total hip replacement. A complete neurologic examination is also needed as neurologic disease would be cause for concern.
Below is a summary of the initial consultation:
– Complete examination
– Sedated X-rays. Most patients (even the best behaved patients) will require sedation for radiographs (x-rays) of the hips. We use these x-rays for measurements of implants, so they must be PERFECT. Remember that the reason your pet is seeing a surgeon is because of hip pain, and the positioning of the x-rays may cause some discomfort, so the kindest way to acquire radiographs is with sedation.
– Blood work: Complete Blood Count (CBC), Chemistry profile, and Urinalysis. This needs to be performed at the MOST 30 days prior to surgery to ensure that your pet is a good anesthetic candidate.
– In older patients, additional diagnostics may be recommended such as chest radiographs and an abdominal ultrasound to get a complete health screen.
Assuming your pet is a good candidate for a total hip replacement the procedure will be described to you in detail along with the potential complications, recovery period/rehabilitation, and overall outcome. If for some reason a total hip replacement is not a good choice or another issue is found, other treatment options will be reviewed in depth. I always mention to owners to allot enough time for the consultation since a lot is performed on that first visit.
Will both hips need a replacement?
Every surgeon may have a differing of opinions on this. My thoughts reflect the more conservative viewpoint of 20% of dogs with disease in both hips, need hip replacements in both hips. We tend to see a large amount of patients compensating very well when one hip is replaced. That being said there are some dogs that do require both be performed. The typical time frame for performing surgery on the second side is about six months (sooner in a small number of patients).
Are there other hip procedures other than a total hip replacement?
There are four main surgeries available for hip dysplasia in the dog. The first two have strict time frame/age requirements. The first is called a Juvenile Pubic Symphodesis (JPS) which is a procedure that fuses a growth plate that allows the acetabulum (cup/socket) to cover the femoral head (ball) better. This must be performed in dogs under 6 months of age, before the growth plate closes on it’s own. The second procedure is called a Double/Triple Pelvic Osteotomy (DPO). This is performed ideally in dogs under 10-12 months of age and prior to development of any arthritis. This procedure improves the coverage of the acetabulum over the femoral head and can be very effective in dogs with subluxation rather than luxations.
The two main surgical interventions for adult dogs with hip dysplasia are the Total Hip Replacement (THR), which is the scope of this article and the Femoral Head Ostectomy (FHO). The femoral head ostectomy is a procedure where the femoral head is removed and not replaced. This removes the painful source of the femoral head as it contacts the surface of the acetabulum. This is performed with a degree of frequency in small breed dogs and cats, but is considered in some cases of larger breed dogs. There are some cases where this procedure is the best option, however it has been seen that overall use and function of the limb is diminished when compared to a successful total hip replacement. In some studies, an unsatisfactory result (decreased range of motion and decreased muscle mass) has been described in as high as 40% of cases where a FHO was performed.
The total hip replacement is a procedure that replaces both the femoral side (femoral head and neck) and the acetabulum. This procedure when successfully performed allows for normal, uninhibited movement of the new hip and generally allows for a full recovery. This procedure has been done in many working dogs (police dogs, service dogs, etc.) in which the dog is able to resume its normal “job”.
Are “cementless” implants better than “cemented” implants?
There are definitely pluses and minuses to both systems. “Cementless” implants are also thought of as press fit and have a surface where the bone grows into the implant. “Cemented” implants are held in place by a polymerizing bone cement and is as strong as it will be once it solidifies and dries. We do see a slightly higher risk of infection around the implants with the cemented implants as well as what is termed “aseptic” loosening. Where the bone anatomy allows, we strive to use the “cementless” implants.
What are the potential risks and complications that could occur after a total hip replacement?
During the initial consultation we always cover potential complications. While the total hip replacement procedure has a high success rate, there are always potential complications. The first type of complication would involve implant complications, which can be exacerbated if the post-operative instructions are NOT strictly followed. Our patients, after all, are dogs and will not regulate their activity appropriately, herein lies the owner’s responsibility. If the patient is too active the more common type of complications are implant shifting, luxation of the hip, fracturing of the femur, femoral stem subsidence, and seroma formation. The first three complication would require another surgery. Other complications could include infection (short and long term), aseptic loosening of the implants, etc.
What is the outcome for my pet after a total hip replacement?
In general, the outcome for the total hip replacement patient is quite good. Ideally the success rate of total hip replacements in the appropriate patient is around 92-95%. The return of function is typically very good and restoration of normal range of motion and improved musculature. The typical recovery/rehabilitation period is about 3 months in total, however it is a gradual ramping up of activity. As I tell my owners, if I can do it with my own dog, you can do it!!
Laryngeal Paralysis
Spring and summer bring about so many good things: the beach, warm weather, family gatherings, to name a few; and then some bad things: bugs, sweltering heat and humidity, allergies, and the list goes on. For your pets, especially your older retrievers and short nosed (brachycephalic) breeds like the pug and bulldog, the heat and humidity can spell danger due to airway conditions. For more information on the brachycephalic dog breathing issues, see my other post http://wp.me/p2vvxS-2R . This article will focus on a condition called laryngeal paralysis which typically affects our large breed dogs, such as the Labrador Retriever and similar breeds, although it has been seen in cats (rarely) and is a defined disease process in horses.
What is laryngeal paralysis?
Laryngeal paralysis can be as bad as it sounds. The larynx is at the back of the mouth and allows the passage of air into the windpipe (trachea). In the video below, it mimics swinging doors and the cartilages (arytenoid cartilage) that form the larynx will open when breathing “in” (inspiration) and open when breathing “out” (expiration). It remains closed during other actions, like eating and swallowing, thus stopping food, water, saliva from going down the trachea. There is a muscle that controls the opening of these cartilages. The muscle (cricoarytenoideus dorsalis muscle) sits on top of the cartilages on both sides and actively contracts to open the cartilages during inspiration. The opening of the cartilages when exhaling is passive as the air blows open the cartilages. Laryngeal paralysis is a condition where the nerves that feed this muscle are not working properly and the muscle atrophies and is nonfunctional – hence the larynx is paralyzed and can’t move normally.
What causes this condition???
In most dogs, we do not know the reason for this condition. We divide the condition into two general types: 1. congenital and 2. acquired. In congenital, this condition is usually seen at an early age and is thought to be hereditary. Some common breeds affected are Siberian Huskies, Bulldogs, Rottweilers, etc. In the second form (acquired), it simply means that the disease occurs secondary from other issues. When we think of causes we have to ask ourselves, what can cause damage/changes to the nerve (recurrent laryngeal nerve) that feeds the cricoarytenoideus dorsalis muscle? Conditions that we evaluate for typically are as follows: cervical (neck) tumors, chest/lung tumors, myasthenia gravis, peripheral neuropathies, previous neck (cervical) trauma, and endocrine diseases. Most of the time, we do not find a direct cause and suspect an undiagnosed peripheral neuropathy as the underlying cause. When we do not know the actual cause we term the disease “idiopathic”. Some recent studies (Stanley, et al) have shown that most (if not all) patients with idiopathic laryngeal paralysis will begin to display some generalized neurologic signs within 1-2 years following the diagnosis.
What are the signs of acquired laryngeal paralysis???
Typically, this affects our larger breed dogs, with the Labrador Retriever being the poster child for this disease. The dogs affected are generally middle to older in age, and either male or female. The most common signs noticed is difficulty breathing, especially when exercising or excited and gagging/coughing when eating/drinking. This is a progressive disease, so signs usually begin with mild changes and become more severe, which can be over months to years. You may also notice a change in the pitch of your dogs bark (voice). Most of the time, we can arrive at a presumptive diagnosis just listening to your pet breathing. As the disease progresses, the affected dog becomes more at risk, and can have a respiratory emergency if not managed appropriately, which can be fatal. Below is a video (the audio is most important) of a dog with laryngeal paralysis:
What diagnostics are involved with laryngeal paralysis???
To begin, a thorough general and neurologic examination is needed for your pet. At minimum, a complete blood work, including a thyroid screening panel, and chest (thoracic) x-rays are needed. The importance of these is to look for other disease processes that may be going on and to ensure that the major organs are functioning appropriately. Why the thyroid panel? Hyopthyroidism (low thyroid hormone production) can cause various neuromuscular issues. With the chest x-rays we are looking for any masses, changes to the esophagus size (megaesophagus) and signs of aspiration pneumonia, which can be seen secondary with laryngeal paralysis. Because most of the patients I see with this condition are older and we are assessing for surgery, I highly recommend an abdominal ultrasound by an experienced ultrasonographer to look for any other concurrent diseases. Bear in mind, if your pet is in a respiratory crisis some of these steps may be done out of order to adequately stabilize the patient.
The best way to confirm the suspected diagnosis of laryngeal paralysis is to look directly at the larynx and assess the functioning of the laryngeal cartilages. This is typically done by inducing a light plane of anesthesia and looking at the back of the mouth. The proper assessment is sort of an art and takes practice to be comfortable making the diagnosis. In addtion to evaluating the larynx, time is taken to look at the rest of the oral cavity for other potential causes. As a surgeon, my preference is to do this examination directly prior to surgery to minimize the amount times the pet needs to undergo anesthesia.
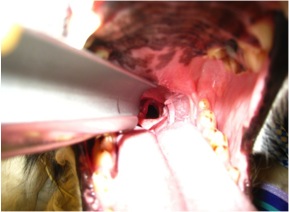
Below is a video demonstrating laryngeal paralysis. The laryngeal opening can be seen and you will notice that it is not moving much at all during the phases of breathing.
How can I treat my pet once laryngeal paralysis is diagnosed???
Probably the better questions is when do I treat? Once a diagnosis is made, then a decision needs to be made. Since this is a progressive disease, if only one side of the larynx is affected then surgical options will most likely be delayed. The most typical treatment for idiopathic laryngeal paralysis is surgical. To date, there is no medical therapy that will restore the function of the larynx. Conservative management will typically incorporate ways to keep your pet cool (air conditioned environment), sedation possibly, and decreasing environmental allergens. If, during our pre surgical diagnostics, we find other issues, changes may be made to the treatment plan. There are some findings that may make your veterinarian reconsider your pet being a good surgical candidate, such as an enlarged esophagus (megaesophagus). The main reason to proceed forward with surgery is to improve your pets quality of life for however long that may be, as well as improve your (as the owner) life by providing more quality time together. There are risks both with surgery and without surgery.
The standard procedure to open the airway is called an arytenoid lateralization (laryngeal tie-back). This is a procedure that pulls one side of the laryngeal cartilages back, permanently opening one side of the larynx. In effect, we override the normal muscular action of the larynx. We gain access to the larynx by an incision made on the side of the neck. None of the work is done within the mouth. There are other procedures that remove the arytenoid cartilage portion of the larynx to permanently open the larynx from within the mouth, called an arytenoidectomy. This procedure, in my opinion, has not been evaluated as much as the “tie-back” procedure.
Below is a picture of an arytenoid lateralization. Notice the difference on the opening from the previous video.
What are the risks with and without surgery and what is the typical outcome?
No procedure is without inherent risks, unfortunately. The risks and benefits of any procedure must always be weighed and discussed with your veterinarian and veterinary surgeon. The most common post-operative complication is aspiration pneumonia. Recent literature cites about a 12-15% risk of aspiration pneumonia following surgery, with the most critical time period being the actual recovery from surgery and the immediate post-operative period. Some medications can be administered that help reduce vomiting, regurgitation and increasing the tone of the lower esophageal sphincter muscle – all aimed at lowering this risk. Most of the time aspiration pneumonia, if caught early, can be treated successfully with antibiotic therapy and supportive care (depending on severity). In a small number of patients, aspiration pneumonia can be fatal. Other complications are break down of the “tie-back” suture and incisional complications such as seroma and abscess/infection. Anesthesia complications can arise with any anesthesia/surgical event, however with proper screening, this risk can be minimized. My feeling is that even dogs prior to a “tie-back” procedure have a higher risk of aspiration pneumonia because the protective mechanism of the larynx is not functioning properly.
Surgically addressing this condition can be life saving and drastically improve the quality of your pets life. Most owners (~90%) are happy they made the decision to proceed forward with surgery and are pleased with the improved quality of life for their pet. If you notice any of these changes to your pet, please plan to see your veterinarian to see if they are a candidate for surgery. While the above article is long, it does not include everything related to this disease, if you have questions, just ask!!!
Kevin Benjamino, DVM, DACVS
Copyright 2015
Meet Faith!!!
Faith is an adult, mixed breed dog that came to Affiliated Veterinary Specialists – Orange Park from a local rescue group (SAFE Pet Rescue) in the Jacksonville, FL area. She was found and brought to a local shelter and had sustained multiple injuries. We suspect that her injuries were most likely caused by being hit by a car. Unfortunately, her injuries are chronic in nature, probably about 4 weeks old and she has learned how to scoot around and pull herself with her front end.
Her major injuries are a right hip luxation and left tibia/fibula fracture. She has normal neurologic function in the hind legs, however she has no support in the back legs……..until surgery. In addition to her orthopedic issues, she also is heartworm disease positive. The decision was made to address the orthopedic conditions in order to get her mobile and then focus on the heartworm disease. The heartworm disease always makes anesthesia more complicated, but with the proper precautions, she did great. Due to the chronicity of the hip luxation, a femoral head ostectomy was performed and the left tibia/fibula fracture was repaired.
Just two days after surgery she is starting to stand on her own and take some steps forward. She is very sweet and has determination. She will make a great addition to someone’s home when she recovered. It is exciting to know that she has been given a well deserved second chance. Please go to the SAFE Pet Rescue website: http://www.safe-pet-rescue-fl.com or following them on Facebook: SAFE Pet Rescue to learn more about Faith and other adoptable dogs!!
Pet Rehabilitation
Check out the new page on http://www.drbenjamino.com
Top 5 List for a Safer Holiday Season
As Halloween and the upcoming holidays are rapidly approaching, we are often wrapped up in family gathering, parties, and other activities and forget about the well being of our beloved pets. I tried compiling a short list to help keep our pets healthy and out of trouble this holiday season. This should ensure that everyone has a happy holiday season and may save you and your pet from needing emergency trips to veterinarian or emergency clinic.
1. Keep candy away from pets, in particular chocolate and candies made with xylitol and other sweeteners. While these taste good, they can have very harmful effects on your pet, ranging from liver failure, seizures, and as severe as death. If you suspect your pet has consumed any of these, seek veterinary care immediately.
2. Keep a close on the whereabouts of your pets. With all the excitement and increased visitors during this time, make sure your pets are accounted for and haven’t run off. Missing pets and subsequent trauma, such as being hit by a vehicle is an all to common occurrence during this time. Make sure your pets are in a safe place when company is over.
3. Keep pets out of the garbage and from grabbing food off the table. Bones and fatty meats can cause illness in our pets, especially dogs. Bones can cause a lot of irritation and in some cases puncture the gastrointestinal tracts. Fatty foods are not good for our pets and can cause pancreatitis and other gastrointestinal issues. Pancreatitis can range in severity and needs to be treated by your veterinarian.
4. Keep cords and electrical wiring away from your pets. Both cats and dogs can find wires enticing. Electrocution injury can be very severe and cause death in some cases. If you believe your pet to have be electrocuted, have them evaluated by your veterinarian immediately.
5. Keep easily ingestible objects away from your pets. Objects that can be easily swallowed can cause gastrointestinal irritation and obstruction. Some objects that can become obstructive are clothes, small toys, tinsel, etc. Gastrointestinal obstructions demand immediate veterinary care. There are times when the object can pass, but most of the time your pet will need surgery to relieve the obstruction, Surgery can range from a single incision in the stomach to removal of a segment of intestine. In extreme cases this condition can be fatal.
October 2014 Case of the Month
October’s case of the month is an interesting one. Lucky is a young chihuahua mix that came to us with SEVERE injuries. He was attacked by a neighborhood dog about 7 days before presenting to us and was in very bad shape. His initial wounds were managed, but unfortunately infection still set in and the majority of his cervical (neck) skin started to die and needed to be removed. Not only was the infection causing a problem locally, but we had signs of it being spread systemically (through his blood stream). He needed both surgical care and care by a criticalist(board certified in Emergency and Critical Care) in order for him to have a fighting chance. Below is a picture of what he looked like when he was admitted into the hospital.
You can make out the extensive injuries on the photo above. He was fortunate to be alive! Whenever we get a case like this (unfortunately it happens more frequently than we like), we am always realistic with the owners, because there is a chance that their pet will not survive. Also, these cases are not quick cases, Lucky was hospitalized for 2-3 weeks and wasn’t fully healed for about 6 weeks. Our first objective is to get the systemic infection under control and get him strong enough to be able to handle surgery. While the criticalist was working on the systemic infection, we were concentrating on the neck wound.
The first phase wounds go through is the debridement phase, which is where the body gets rid of necrotic (dead) tissue and the size of the wound is established. The next phase to follow is the granulation phase. The granulation phase is very important in a large wound like this, this is when the body begins to infiltrate the wound with healthy tissue and more importantly capillary vessels, which bring blood flow. For this wound, I choose to use a wound dressing called BurnStat (Ubuntu) which is a dressing that can be used through multiple phases. It is an organic clay substrate that does an excellent job of removing toxins and necrotic tissue while promoting granulation tissue formation.
Following this type of bandaging, the diseased tissue begins to be replaced with more healthy, red granulation tissue. The final product, before being able to close the wound, needs to be completely covered with granulation tissue in order to increase the chance of the new skin being accepted.
You can see how the surface is covered with healthy looking tissue and no presence of dying tissue visible. By this time Lucky amazingly over came his battle with the widespread infection and overall was doing very well. He was making a remarkable recovery.
Our next dilemma was “how do we cover the exposed tissue”? In cases like this, we have a few options, which is beyond the scope of this post. I choose to use an advancement flap (skin freed up from a nearby location that is moved over the wound), which made the most sense due to the elasticity of the skin in this area. Below is his wound following surgery.
Following surgery we also utilized laser therapy to help promote uptake of the skin flap. This is Lucky in his referee uniform (it is close to Halloween) receiving his laser therapy.
Here is the finished product for Lucky!!! He overcame a lot of obstacles along the way!!
September 2014 Case of the Month – Meet Tido!!!
Meet Tido!!! Tido is a 6 1/2 year old West Highland White Terrier that came to us (Affiliated Veterinary Specialists – Orange Park) for a lower esophageal foreign body. He started showing signs of intermittent vomiting and regurgitation after swallowing his rawhide bone. Unfortunately, it became lodged in the portion of the esophagus that goes through his chest, just past his heart. Usually we can use a scope camera and remove the object without any incisions. The piece of rawhide was wedged in this area and was unable to be moved, so surgery was his only option.
An incision was made in the chest and the large piece of rawhide was found in the esophagus just past the heart. An incision was made into the esophagus and the rawhide was removed. Surgery on the esophagus is a very delicate surgery. In this area we have big vessels (aorta) above the esophagus and the vena cava below. Just in front of the esophagus is the heart. Nearby, there are very important nerves (vagus) that course over the esophagus. Also, the esophagus has a harder time healing versus other areas of the gastrointestinal tract with a higher chance of stricture (narrowing due to scar tissue) formation.
After the rawhide was removed, the esophagus was closed in two layers and then a Vetrix Extracellular Matrix (ECM) sheet was placed. This will aid in healing by providing a scaffold for the tissue to heal and incorporate the bodies own stem cells to infiltrate the area. After the esophagus was closed, Tido’s chest was closed in a standard fashion.
Tido made an excellent recovery!!! He has been on a soft diet and no rawhides for him!!! In four weeks he should be able to resume his normal activity. At his two week recheck, you could never tell he had surgery. Way to go Tido!!!
February 2014 Case of the Month – Meet Smokey!!!

Smokey at his two week recheck!
Smokey was transferred to the surgery department from the overnight emergency service after being attacked by a larger dog the night before. His injuries were multiple and severe. He sustained multiple bite wounds over his thoracic and abdominal body cavities. Thoracic radiographs revealed multiple left sided rib fractures and multiple defects (tears) into the chest wall. The bite wounds over the abdomen were superficial with no evidence of penetration in the abdomen.
Smokey was stabilized by the emergency service and prepared for surgery once transferred in the morning. Based on the injuries, Smokey had a thoracic exploratory to evaluate the thoracic wall wounds and subsequent internal injuries. Surgery revealed a large thoracic wall defect and multiple fragmented ribs, some of which needed to be removed. Interestingly, the left caudal (posterior) lung lobe had a large laceration caused by one of the rib fragments, necessitating removal of the lung lobe. The remaining thoracic wall defect was too large to close primarily.

The white arrow denotes the diaphragm, the red arrow is showing the muscle of the thoracic wall and the caudal edge of the heart and the black arrow denotes the great vessels (caudal vena cava and caudal aorta).
The thoracic wall defect was repaired using porcine small intestinal submucosa extracellular matrix sheets (Vetrix ECM). Note the placement of the ECM in the defect. The overlying muscle was freed and placed as a muscular flap over the ECM. Following the repair a thoracic tube was placed to maintain negative pressure in the chest following surgery. Smokey recovered well from surgery and was released 48 hours following surgery. Two weeks later at his suture removal and he is doing great!