Primary lung tumors are cancers that we as veterinarians see with less frequency than in human medicine, when we are both looking for them and when we are not looking for them. What I mean by that statement is sometimes the patient (dog or cat) may be displaying signs associated with a tumor in the lungs and sometimes they are not and we find them during routine chest radiographs (x-rays). While lung cancer generally conjures up a visceral negative reaction in most people, many primary lung tumors can be managed successfully giving the patient a good quality of life for some time. We do find that dogs tend to have a better prognosis with primary lung tumors than do cats, unfortunately. What do I mean by primary lung tumor? A primary lung tumor is a tumor originating within the lung tissue that is the sole tumor versus metastatic nodules within the lungs, which are smaller tumors scattered in the lung due to a tumor originating from another organ.
What are signs of a lung tumor?
Unfortunately, many primary lung tumors do not have associated signs and we find them by chance if we are looking in the chest. The good and bad is that we would always prefer to provide treatment (surgery) in a patient that does not have signs, however the bad part is that these tumors can get very large before seeing signs. The most common signs seen are respiratory symptoms including coughing, exercise intolerance, excessive panting for a variable duration of time and variable frequency. Very rarely will a patient present with blood, fluid, or air in their chest due to the tumor. More infrequent would be presenting with a condition called hypertrophic osteopathy – swelling and pain in limb(s) related to a lung tumor.
How do we diagnose a lung tumor?
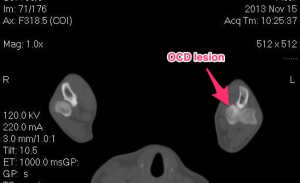
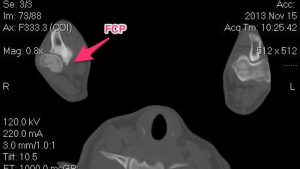
The typical way to diagnose a primary lung tumor is with radiographs (x-rays) of the chest. If a large solitary mass is seen, it is suspected to be a primary lung tumor. Another was to visualize a primary lung tumor would be to perform a CT (computed tomography) scan of the chest. A CT scan gives us excellent detail of the mass and allows a very in depth view of the rest of the lung tissue for evaluation. Some advocate for a fine needle aspirate of the mass (sticking an needle in the mass to get a representative sample of cells) prior to discussing surgery. Typically a solitary lung mass will be a pulmonary adenocarcinoma and a fine needle aspirate will only yield a diagnostic result only 60-70% of the time. Many believe (myself included) that surgery is the next step for a diagnosis. Prior to surgery a minimum staging database should be acquired. This includes (in addition to chest x-rays and/or chest CT scan) complete bloodworm with urinalysis and an abdominal ultrasound (or contrast CT scan). This is to evaluate body organ function and the presence of metastasis or other non-related issues, since most patients with a primary lung tumor fall into the geriatric age category, it is not uncommon to uncover other issues.
What is the treatment for a primary lung tumor?
The standard treatment for a primary lung tumor is surgical removal. At this juncture (or earlier) your primary veterinarian may recommend that you consult with a board certified veterinary surgeon due to the intricacy of the procedure and the “around the clock” care your family member will require following surgery (if your veterinarian does not offer this service). Generally, surgical removal of the tumor is the standard of care for treatment of this disease. Smaller tumors can sometimes be removed by thoracoscopy (minimally invasive scoping of the chest), however a very experienced anesthesia team is need to provide one lung lobe ventilation to the pet. Usually the tumor is accessed by a lateral thoracotomy depending on the which side of the chest the tumor is located. The tumor is isolated and the affected lung lobe is removed (various techniques can be used). I prefer removal with a Thoracoabdominal (TA) stapling device. In all surgeries, a chest tube is placed for 12-24 hours following surgery.
What type of cancer is a primary lung tumor?
The most common tumor type is a pulmonary adenocarcinoma in both the dog and cat. When a histopathology report is generated, we usually look to see whether the tumor is well-differentiated or poorly differentiated, which can give us some indication regarding the metastatic nature of the tumor. Other types of tumors such as squamous cell carcinomas, sarcomas and benign tumors are very rare.
What is the prognosis for a primary lung tumor?
The information on cats and prognosis after removal of a primary lung adenocarcinoma is limited, however the results seem to be not as favorable for this species. Also, the survival rate is very dependent on whether there is any sign of metastasis (lymph node involvement, nodules elsewhere, malignant effusion (fluid) in the chest and/or abdomen). In some reports, cats with signs of metastasis following surgical removal have a survival rate of < 3weeks.
Dogs with this disease tend to have a much more favorable prognosis with >50% of dogs with a solitary lung tumor (no metastasis) living > 1 year following surgery with good quality of life. Factors that can change our prognosis include large size of tumor, lymphatic involvement, pleural effusion, etc.
I always encourage my clients to speak with a board certified veterinary oncologist about follow-up care for these patients. More and more we are finding that we may be able to extend our pets quality of life with various chemotherapy options by slowing the recurrence or spread of disease following surgery.
Authored by:
Kevin Benjamino, DVM, DACVS
Copyright 2015